Non-Invasive Neurostim Insurance: What’s Covered and What’s Not?
At NeuroTechInsider.com, we’re all about cutting through the noise when it comes to brain wellness and sleep tech. Whether you’re eyeing a vagus nerve stimulator, a transcranial magnetic stimulator, or a wearable migraine relief band, knowing what your insurance actually covers is a game-changer. No one wants to drop hundreds (or thousands) of dollars on a device only to find out it’s not reimbursable.
In this guide, we’ll walk you through the complex world of non-invasive neurostim insurance—what gets covered, what doesn’t, and how to boost your chances of getting approved.
What Is Non-Invasive Neurostimulation?
Non-invasive neurostimulation refers to devices that stimulate the nervous system externally—without requiring surgical implantation. These devices deliver electrical, magnetic, or acoustic pulses to modulate brain or nerve activity, offering relief from:
- Chronic pain
- Migraines
- Depression
- Insomnia and stress
Unlike pharmaceuticals, neurostim devices aim to support natural neurological function. And with evidence stacking up in their favor, insurance providers are slowly starting to take notice—though coverage is still patchy at best.
“Insurance policies often lag behind medical innovation. Just because a device works doesn’t mean it’s covered.”
Let’s break down the most common non-invasive devices and how insurers treat them.
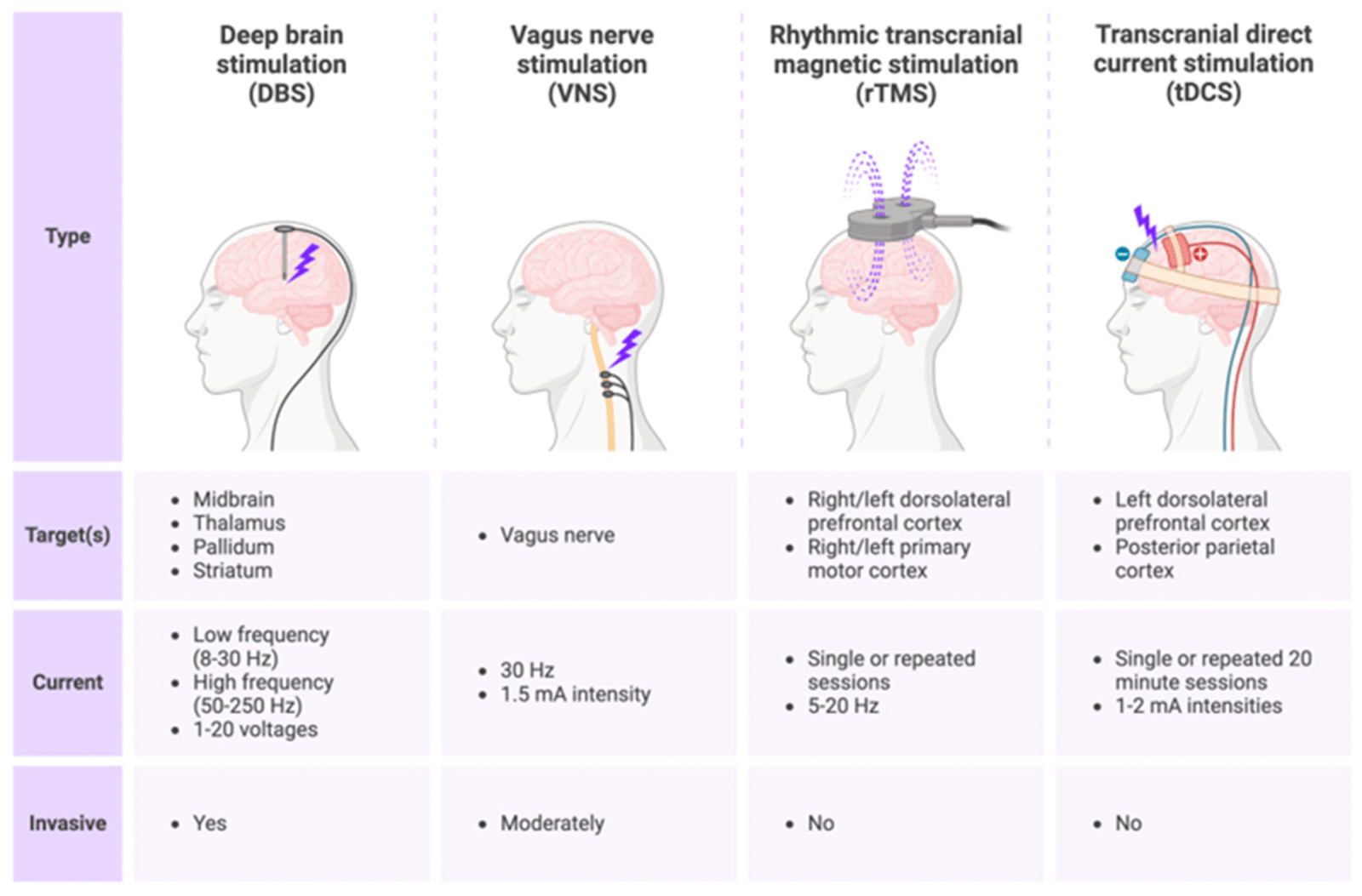
Types of Non-Invasive Neurostim Devices
There are several categories of non-invasive neurostimulators on the market today. Each one varies in how it works, what it treats, and how insurance classifies it.
TENS – Transcutaneous Electrical Nerve Stimulation
TENS devices are among the most widely accepted. They’re FDA-cleared for managing pain, especially post-operative and chronic musculoskeletal pain. Because of their long history, they’re often covered under Durable Medical Equipment (DME) policies.

- ✅ Commonly reimbursed when prescribed post-surgery
- ❌ Rarely covered for alternative uses like migraine or stress relief
If you’re exploring TENS options for mood or sleep regulation, chances are you’ll have to pay out-of-pocket—or appeal a denial.
eTNS – External Trigeminal Nerve Stimulation (e.g., Cefaly)
Designed primarily for migraine relief, eTNS devices like Cefaly stimulate the trigeminal nerve externally. While clinical results have been promising, most insurance providers still categorize these devices as “experimental” or “wellness” tools.
- ❌ Generally not covered by insurance
- ✅ Often available over-the-counter without a prescription
That said, some progressive employers and flexible spending plans might reimburse OTC neurostim purchases. It’s worth checking your FSA/HSA guidelines.
TMS – Transcranial Magnetic Stimulation
TMS therapy is FDA-approved for treatment-resistant depression and is widely accepted in clinical psychiatry. This technology uses magnetic fields to stimulate areas of the brain linked to mood regulation. Devices like NeuroStar are often delivered in a clinical setting by a licensed psychiatrist.
- ✅ Often covered by Medicare and commercial insurance for major depressive disorder (MDD)
- ⚠️ Requires documentation of failed antidepressant treatments
- ⚠️ Usually needs prior authorization
This is the gold standard for neurostimulation insurance coverage—but only if you meet the criteria. At NeuroTechInsider, we’ve reviewed at-home alternatives like Apollo Neuro and NeuroVIZR, but these aren’t covered as clinical-grade TMS is.
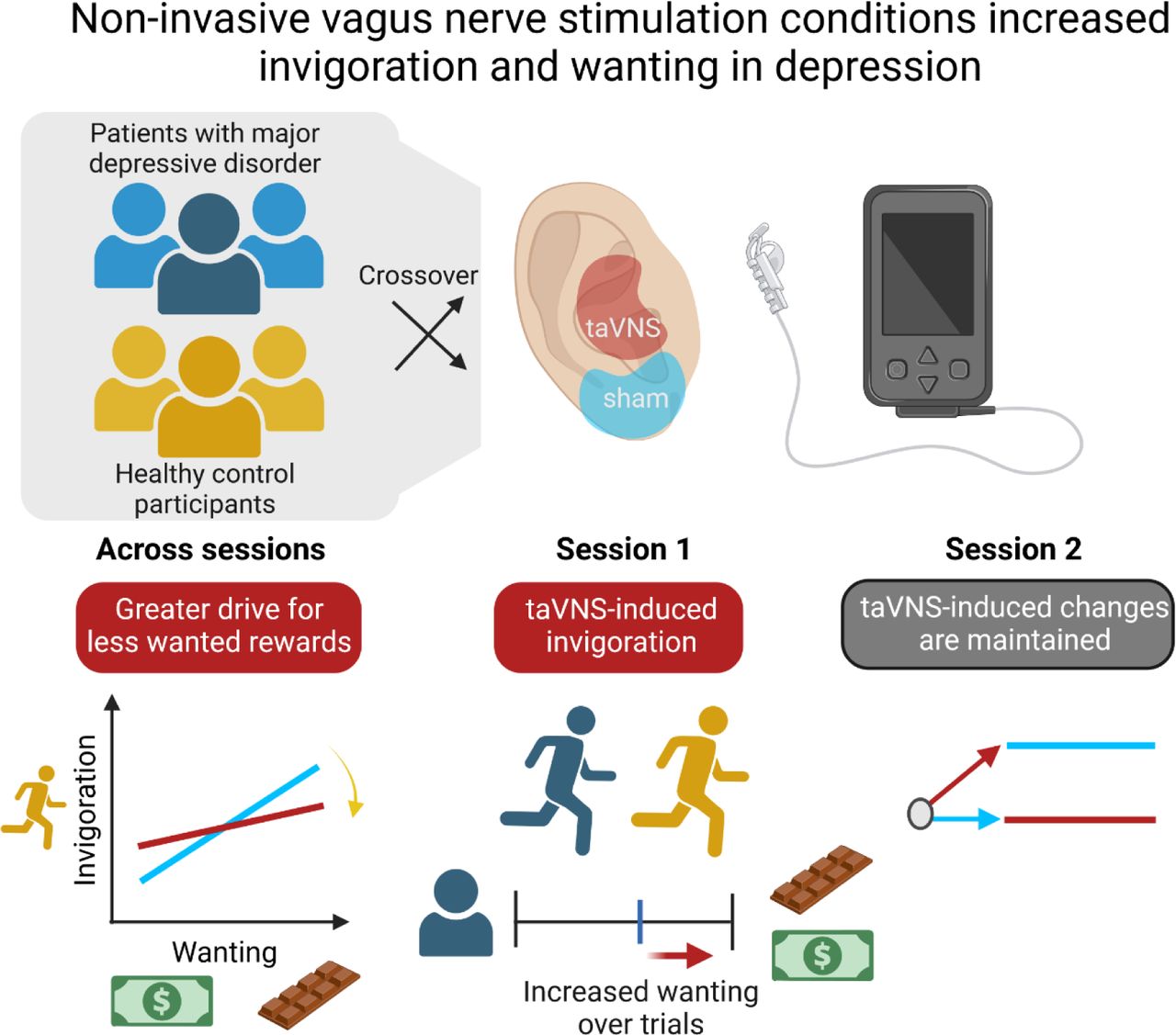
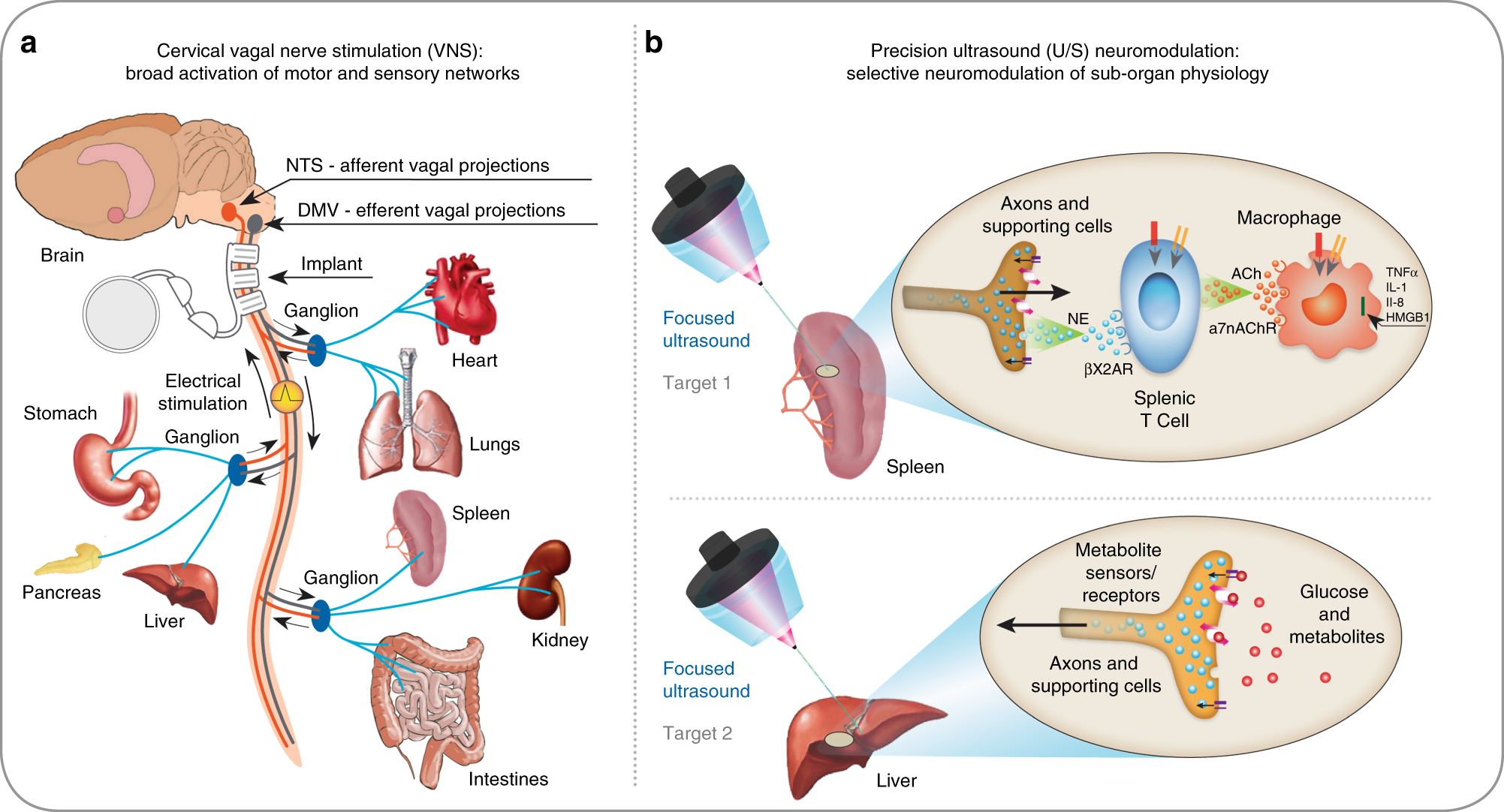
nVNS – Non-Invasive Vagus Nerve Stimulation (e.g., gammaCore)
nVNS devices like gammaCore are gaining traction for managing cluster headaches, migraines, and even anxiety. These stimulate the vagus nerve through the neck using electrical impulses.
- ❌ Rarely covered by insurers
- ⚠️ Some Medicare plans may classify them as TENS (DME loophole)
- ✅ Supported by VA for headache and pain relief
Coverage here is all about classification. If your provider or insurer sees it as a TENS variant, you might get lucky. Otherwise, expect to appeal or self-pay.
REN – Remote Electrical Neuromodulation (e.g., Nerivio)
REN devices like Nerivio deliver electrical pulses via the upper arm, targeting migraine pathways through remote modulation. It’s a unique and growing segment.

- ❌ Not covered by Medicare
- ❌ Commercial coverage rare but may improve as clinical data evolves
Despite strong early evidence, REN is still considered “too new” by many payers. That said, you can often apply manufacturer coupons or patient assistance programs to reduce cost.
Does Insurance Cover Neurostim Devices?
Short answer? Sometimes. Coverage varies drastically depending on:
- Your insurance provider
- Your diagnosis and medical history
- The specific device you’re using
- FDA clearance and evidence backing the device
Let’s break it down by insurer type.
Veterans Affairs (VA)
The VA tends to be more progressive in device coverage. They often approve FDA-approved tools like TENS, TMS, and even nVNS for veterans dealing with chronic pain, PTSD, and migraines.
Medicare & Medicaid
Medicare classifies most external neurostimulators as DME, which means:
- You can get reimbursed for basic TENS use
- You may hit caps on device pricing and replacement timelines
- REN and newer devices are excluded
Some Medicaid programs at the state level may approve neurostim devices if medically necessary, but this is rare and very case-by-case.
Commercial Insurance Providers
This is where things get messy. Some commercial plans, like Aetna or BlueCross, may cover TMS or TENS but deny newer options like nVNS or REN—even when backed by clinical research.
They often cite lack of long-term efficacy data or label the tech as “experimental.” That’s why documentation and pre-authorization are key—which we’ll cover next.
Documentation and Medical Necessity: How to Get Covered
Want to increase your chances of getting insurance to pay for your neurostim device? You’ll need more than just a doctor’s note. Most insurers require proof that:
- You’ve tried and failed conventional treatments (like meds or therapy)
- Your condition is clinically diagnosable and persistent
- You’ve got documentation from a specialist—not just a general practitioner
Insurance companies want a paper trail. And that means you need to come prepared with the right materials.
Essential Documents for Approval
- Physician’s Statement – Ideally from a neurologist, psychiatrist, or pain specialist
- Clinical Notes – Include DSM-5 or ICD-10 diagnosis codes
- Prior Treatment History – Antidepressants, migraine meds, therapy attempts
- Device Prescription or Recommendation – Signed by your provider
- Insurance Prior Authorization Form – Provided by your insurer
“The more specific the medical necessity claim, the better. Vague or generic letters will almost always get denied.”
Many device manufacturers like NeuroStar or gammaCore offer assistance programs to help your provider with pre-auth paperwork. Use them.
How to Check Your Neurostim Coverage
If you’re not sure what’s covered, here’s a step-by-step method to find out without making 10 phone calls or going down a Reddit rabbit hole.
Step-by-Step Coverage Check:
- Review your plan – Look under “Durable Medical Equipment,” “Behavioral Health,” or “Alternative Therapies.”
- Search for keywords like “TENS,” “TMS,” or “neurostimulation.”
- Call the customer support line – Ask specifically: “Is device X covered for condition Y?”
- Ask about prior auth – Get the form and fax instructions.
- Talk to your doctor or neurologist – Share everything you learned and have them submit.
If you get a “no,” don’t give up. This is where appeals come in.
What If You’re Denied?
Insurance companies often deny first attempts—not because they don’t work, but because you didn’t follow their rules. Here’s what you can do:
- Submit an appeal with detailed justification
- Include peer-reviewed studies like this one on TMS efficacy for depression
- Reference FDA approvals for the device
- Ask your provider to write a stronger letter emphasizing your history
Some patients also find success through patient advocates or lawyers, especially for long-term coverage battles.
Quick Comparison Table: Insurance Coverage by Device
| Device | VA | Medicare | Commercial |
|---|---|---|---|
| TENS | ✔️ | ✔️ (limited) | Varies |
| eTNS (Cefaly) | ✔️ | ❌ | ❌ |
| TMS (NeuroStar) | ✔️ | ✔️ | ✔️ (with criteria) |
| nVNS (gammaCore) | ✔️ | ❌ | ❌ |
| REN (Nerivio) | ❌ | ❌ | ❌ |
Final Thoughts: Can You Rely on Non-Invasive Neurostim Insurance?
Let’s be real—insurance coverage for neurostim devices is still the Wild West. While clinical tools like TMS are gaining traction, most wearable or consumer-grade devices still fall outside the approval zone. But that doesn’t mean you should count them out.
If you’re exploring options like Apollo Neuro, Sensate, or NeuroVIZR for stress and focus, these likely won’t be covered—yet. But the science is moving fast, and so is policy.
As always, advocate for yourself. Get the documentation, ask the right questions, and lean on your doctor’s support. And if your insurer says no, fight back. People win appeals every day.
What to Do Next:
- Download a free prior authorization template
- Read our neurostimulator comparison guide
- Sign up for updates on FDA approvals, insurance news, and product deals
And remember: if you’re investing in your brain, you deserve to know what’s possible—not just what’s covered.
FAQs: Non-Invasive Neurostim Insurance
Is TMS therapy covered by most insurance plans?
Yes, especially for major depressive disorder that hasn’t responded to medication. Medicare, VA, and many commercial insurers approve it with pre-authorization.
Are devices like Apollo Neuro or Sensate covered?
Not currently. These are considered consumer wellness tools, not medical devices. But you may use FSA/HSA funds to purchase them.
What can I do if my claim is denied?
You can appeal by submitting additional clinical justification, provider documentation, and peer-reviewed research backing the device’s use for your condition.
Does the VA offer more comprehensive neurostim coverage?
Yes. Veterans Affairs is often more flexible, especially for pain and mental health conditions. Devices like TENS, TMS, and nVNS are regularly approved through VA healthcare.
NeuroTechInsider.com is your trusted guide in navigating brain tech. We’re here not just to review—but to empower. Join the future of non-invasive neurowellness, with science and strategy on your side.
https://pub.mdpi-res.com/biosensors/biosensors-14-00335/article_deploy/html/images/biosensors-14-00335-g002.png?1720663545