Understanding the Sleep Disorder Diagnosis Process
Getting a good night’s sleep is essential for overall health and well-being. But when sleep becomes elusive, it may be more than just a bad night. **Sleep disorders** affect millions of people worldwide, from conditions like **insomnia** to **sleep apnea** and **narcolepsy**. Diagnosing a sleep disorder involves a comprehensive process that can involve clinical evaluations, sleep logs, questionnaires, and a series of specialized tests. If you’re struggling with sleep issues, understanding the steps involved in the diagnosis process is critical to finding the right treatment.
In this article, we break down the **sleep disorder diagnosis process**, explaining each step involved, from initial consultations to diagnostic tests, and the treatment planning that follows. With the right diagnosis, patients can receive tailored treatments that improve their sleep quality, health, and overall quality of life.
What is Sleep Disorder Diagnosis?
**Sleep disorder diagnosis** refers to the process used by healthcare professionals to identify specific conditions that affect sleep. Sleep disorders are conditions that cause disturbances in the way people sleep, such as difficulty falling asleep, staying asleep, or experiencing restful sleep. These disorders can significantly impact mental health, physical health, and overall productivity.
There are various types of sleep disorders, including:
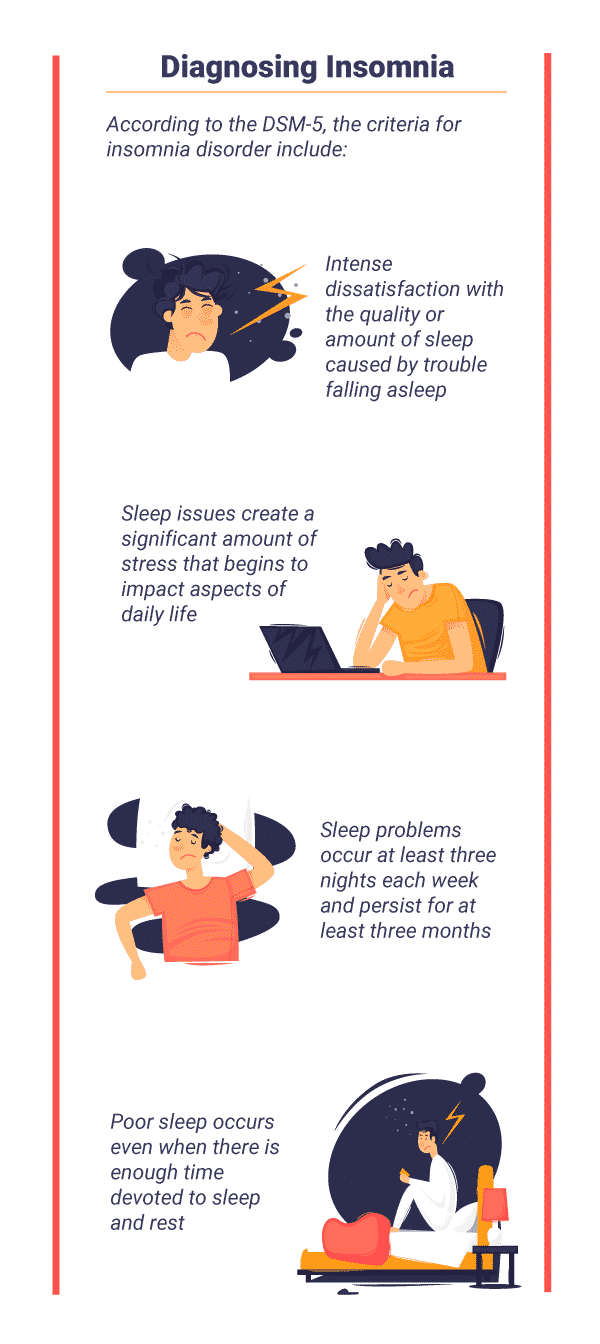
- Insomnia: Difficulty falling or staying asleep.
- Sleep Apnea: A condition where breathing repeatedly stops and starts during sleep.
- Restless Leg Syndrome (RLS): A strong urge to move your legs, usually at night, which disrupts sleep.
- Narcolepsy: A condition characterized by excessive daytime sleepiness and sudden sleep attacks.
It’s important to note that sleep disorders can sometimes be related to other health issues like anxiety, depression, or neurological conditions. This makes it essential for a healthcare provider to conduct a comprehensive evaluation before arriving at a diagnosis.
Why Accurate Diagnosis is Crucial
Accurately diagnosing a sleep disorder is crucial for several reasons. Not only does it help in identifying the underlying cause of the symptoms, but it also ensures that the treatment provided is effective. Without a correct diagnosis, patients may receive treatments that don’t address their specific condition, potentially leading to worsening symptoms or unnecessary side effects.
For instance, if a person with **insomnia** is incorrectly diagnosed with **sleep apnea**, they may be prescribed a treatment like CPAP therapy that doesn’t target their actual problem. This misdiagnosis could delay getting the right care. For more on the importance of accurate sleep disorder diagnosis, read more on Sleep Foundation.
Step 1: Clinical Evaluation
The first step in diagnosing a sleep disorder is a thorough clinical evaluation. This typically begins with a review of the patient’s **medical history** and **sleep patterns**, followed by a **physical examination** to rule out other health issues.
Medical and Sleep History
The healthcare provider will ask detailed questions about the patient’s sleep habits, such as the time it takes to fall asleep, the frequency of nighttime awakenings, and the overall quality of sleep. It’s common for patients to be asked to keep a **sleep diary** for a few weeks to track their sleep patterns and any sleep disruptions they experience.
Additionally, **input from a bed partner** can provide valuable information. For instance, if a person is experiencing snoring or unusual movements during sleep, this may suggest a condition like **sleep apnea** or **restless leg syndrome**. Understanding the full scope of the problem is key to getting an accurate diagnosis.
Physical Exam
A physical exam helps the healthcare provider assess whether there are any **underlying health conditions** that could be contributing to the sleep issue. For example, a person with thyroid problems may experience symptoms that overlap with sleep disorders like insomnia. The doctor may check for other conditions that could interfere with sleep, such as obesity, which is a common risk factor for **sleep apnea**.
Step 2: Sleep Logs and Questionnaires
Once the clinical evaluation is complete, the next step involves using sleep logs and questionnaires to gain further insight into the patient’s sleep patterns and behaviors. These tools help healthcare providers assess the severity of the sleep disorder and identify specific symptoms.
Sleep Diary: Tracking Your Sleep Patterns
A **sleep diary** is an essential tool in diagnosing sleep disorders. It allows the patient to track their bedtime, wake time, and the quality of sleep over a period of time, typically 1-2 weeks. This record helps to pinpoint patterns or triggers that may be contributing to the sleep problems.
Here’s what a typical sleep diary might include:
- Time you went to bed and woke up
- Time it took to fall asleep
- Any nighttime awakenings
- Feelings upon waking (e.g., refreshed or groggy)
- Any sleep disturbances (e.g., snoring, leg movements)
By analyzing this data, healthcare providers can identify potential issues such as poor sleep hygiene, insomnia, or other more complex disorders like **sleep apnea**.
Sleep Questionnaires
Step 3: Diagnostic Tests for Sleep Disorders
If the clinical evaluation and questionnaires suggest that a sleep disorder is present, the next step may involve more detailed **diagnostic tests** to confirm the condition. These tests are typically used to evaluate conditions like **sleep apnea**, **narcolepsy**, and **restless leg syndrome**. They help gather objective data about the patient’s sleep and provide a clearer picture of what is happening during the night.
Polysomnography (PSG)
**Polysomnography (PSG)** is an overnight sleep study that takes place in a specialized sleep lab. This test monitors multiple body functions while the patient sleeps, including **brain waves**, **heart rate**, **breathing patterns**, and **muscle activity**. PSG is particularly useful for diagnosing conditions like **sleep apnea**, **narcolepsy**, and **parasomnias**.
During the test, electrodes are attached to the scalp and other parts of the body to monitor the various physiological functions. The data gathered from PSG can reveal the presence of sleep disorders that may not be obvious during a regular clinical evaluation.
For more information on how **PSG** works, check out this Sleep Foundation article on Polysomnography.
Home Sleep Apnea Test (HSAT)
For patients suspected of having **sleep apnea**, a simplified version of the PSG called the **Home Sleep Apnea Test (HSAT)** may be used. HSAT can be done at home, where the patient wears a small device that records breathing patterns and heart rate during sleep. This test is particularly effective in diagnosing **obstructive sleep apnea (OSA)**.
HSATs are less comprehensive than PSG but are often a good option for patients with symptoms that suggest sleep apnea, such as heavy snoring or excessive daytime sleepiness.
Conclusion
Accurate diagnosis is the first step in effectively treating **sleep disorders**. If you’re experiencing symptoms like difficulty falling asleep, frequent awakenings, or daytime fatigue, understanding the diagnosis process can help you take control of your health. Early detection and treatment can make a significant difference in improving sleep quality and overall well-being.
Don’t let sleep problems continue to affect your life. Start by consulting a healthcare provider who can guide you through the diagnostic process and help you find the right treatment for your sleep disorder.
Step 4: Additional Steps for Accurate Diagnosis
In some cases, the initial clinical evaluation, questionnaires, and sleep logs may not provide a clear diagnosis. This is where **additional steps** come into play. These include **bed partner observations** and reviewing the patient’s lifestyle and medication use, which can provide crucial insights into the underlying cause of sleep disturbances.
Bed Partner Observations
Many sleep disorders, especially **sleep apnea**, involve behaviors that occur during sleep, such as snoring, gasping for air, or abnormal body movements. If you have a **bed partner**, their observations can be invaluable in diagnosing these conditions. Bed partners are often the first to notice signs of **sleep apnea** or **restless leg syndrome**, which can be difficult for the person experiencing them to recognize.
If your bed partner notices any of these signs, it’s important to mention them to your healthcare provider. This extra layer of information can help with the diagnostic process and improve treatment planning.
Review of Medications and Lifestyle Factors
**Lifestyle factors** such as diet, exercise, and stress levels can significantly impact sleep quality. Caffeine, alcohol, and nicotine use can disrupt sleep, and understanding your daily habits is an important part of the diagnostic process. **Medications** may also play a role in sleep problems—certain drugs can cause side effects that interfere with sleep or cause drowsiness during the day.
By reviewing your medications and lifestyle, healthcare providers can determine if these factors are contributing to the sleep disorder or if they need to be addressed as part of the treatment plan.
Step 5: Diagnosis and Treatment Planning
Once all the necessary tests and evaluations are complete, the healthcare provider will work with you to **diagnose** the sleep disorder and develop a tailored treatment plan. This plan will depend on the specific condition diagnosed, and treatment options may vary accordingly.
Treatment Options for Sleep Disorders
Depending on the type and severity of the sleep disorder, several treatment options may be considered. Here are some of the most common treatments:
- Behavioral Therapy: Cognitive Behavioral Therapy for Insomnia (CBT-I) is a well-researched approach that helps people with insomnia change their thought patterns and behaviors around sleep.
- Continuous Positive Airway Pressure (CPAP): For sleep apnea, a CPAP machine is often recommended. This device delivers a steady stream of air to keep the airway open during sleep.
- Medications: Medications may be prescribed to treat specific sleep disorders. For example, **sedatives** or **sleep aids** can help with insomnia, while **stimulants** may be used for **narcolepsy**.
- Lifestyle Changes: Improving sleep hygiene by adjusting bedtime routines, eliminating caffeine intake before bed, and creating a calming sleep environment can make a significant difference in managing many sleep disorders.
For more information on **treatment options** and what might be best for your situation, check out our in-depth guide on Sleep Foundation Treatments.
Conclusion: Taking the First Step Towards Better Sleep
Diagnosing a **sleep disorder** is a critical first step in addressing the root cause of sleep disturbances. With the right tests, evaluations, and professional guidance, you can receive a proper diagnosis and begin a treatment plan tailored to your specific needs. Early detection and accurate diagnosis can significantly improve your quality of sleep and overall health, leading to better energy, mood, and performance throughout the day.
If you’re struggling with sleep issues, don’t hesitate to consult a healthcare provider. With advances in diagnostic techniques, including **Polysomnography**, **Home Sleep Apnea Tests**, and **actigraphy**, we can get closer to understanding your sleep challenges and finding the most effective solution. So, take control of your sleep and your life today. The right treatment starts with the right diagnosis.
Remember, you don’t have to go through this alone. The right support, tools, and knowledge are available to guide you every step of the way.
FAQs: Sleep Disorder Diagnosis
What are the most common sleep disorders?
The most common sleep disorders include **insomnia**, **sleep apnea**, **restless leg syndrome (RLS)**, and **narcolepsy**. These disorders can lead to poor sleep quality, fatigue, and a variety of other health issues.
How is sleep apnea diagnosed?
**Sleep apnea** is typically diagnosed through **Polysomnography (PSG)**, a sleep study that records brain waves, heart rate, and breathing patterns while you sleep. Alternatively, a **Home Sleep Apnea Test (HSAT)** may be used for diagnosing obstructive sleep apnea at home.
What should I expect during a sleep study?
During a **sleep study**, you will be monitored overnight in a sleep lab. Various sensors will be attached to your scalp, face, chest, and legs to track brain waves, heart rate, breathing, and muscle activity. This data helps diagnose conditions like **sleep apnea** and **narcolepsy**. It’s a painless procedure that allows healthcare providers to get detailed insights into your sleep patterns.
Can lifestyle changes help treat sleep disorders?
Yes, **lifestyle changes** such as establishing a consistent bedtime routine, eliminating caffeine before bed, and creating a calm, dark sleeping environment can significantly improve sleep quality and help manage conditions like **insomnia**. Additionally, regular exercise and stress reduction techniques can promote better sleep.
Is sleep disorder treatment covered by insurance?
Many treatments for **sleep disorders**, including sleep studies and CPAP therapy, are often covered by health insurance. However, coverage may vary depending on the insurance plan. It’s best to check with your insurance provider to understand the details of your coverage.
For more detailed information on the **diagnosis** and treatment of sleep disorders, visit [NeuroTechInsider](https://neurotechinsider.com) for expert reviews on the latest **neurostimulation devices** that may complement your treatment plan.